Introduction
Amelogenesis imperfecta (AI) is a hereditary disorder expressing group of conditions that cause developmental alterations in the structure of enamel. A complex inheritance pattern gives rise to amelogenesis imperfecta(AI), a structural defect of tooth enamel.[1]
Generally both the primary and permanent dentitions are involved diffusely. Various causes of amelogenesis imperfecta include febrile illness or vitamin deficiency, local infection or trauma, fluoride ingestion, congenital syphilis, birth injury, premature birth or idiopathic factors.[2]
Broadly, amelogenesis imperfecta has been categorized into four groups primarily based on phenotype—hypoplastic, hypocalcified, hypomaturation, and hypomaturation-hypoplastic with taurodontism[3].
Chief problems in amelogenesis imperfect include poor dental esthetics as there is abnormal enamel formation and abnormal color of teeth: yellow, brown or grey, reduced vertical dimension and teeth sensitivity[4],[5]
Various other dental anomalies which are associated with amelogenesis imperfecta are multiple impacted teeth, congenitally missing teeth, hypercementosis, root malformation, and taurodontism.[6],[7],[8] Anterior open bite with posterior deep bite may occur.[9]
Clinical manifestations vary in affected males as well as females. In the hypoplastic form, females show vertical ridging of the enamel, whereas, there is uniform hypoplasia in males. In the hypomaturation form,[10],[11] males present with irregular pigmented mottling whereas females present with vertical bands of mottling which is inconspicuous under normal light conditions which is known as lyonization.[12],[13],[14]
Restoration of these defects is important not only because of esthetic and functional concerns, but also because there may be a positive psychological impact for the patient.[15],[16],[17]
Treatment planning for patients with amelogenesis imperfecta is related to many factors:
Intraoral condition, the age and socioeconomic status of the patient, the type and severity of the disorder.[18],[19] Patients have been known for trying so many things to cover their teeth with pieces of paper, chewing gum or other materials in order to mimic an "ordinary" appearance. Many young people with AI request the removal of their teeth and the fitting of dentures in a society where having one's own teeth is the longed-for norm.
Also, a carefully designed and executed temporization phase is vital for overall treatment success, particularly for severe cases that require extensive rehabilitation. Since amelogenesis imperfecta is often complicated with occlusal disharmony, reduced vertical dimension and limited interocclusal clearance, so it usually requires establishment of a new occlusion.
This case report demonstrates a sequenced and logical approach to treat a patient having marked tooth damage caused by amelogenesis imperfecta.The treatment for amelogenesis imperfecta is mainly aimed on esthetic and functional rehabilitation. Moreover, careful planning with adequate follow up enabled the patient to attain satisfactory results.
Case Report
A 32-year-old female patient presented in the O.P.D of Prosthodontics at the Himachal institute of dental sciences, Paonta Sahib with a chief complaint of discoloured and malformed teeth including size, shape and shade of her teeth. Medical history was noncontributory. Extraoral examination did not reveal any relevant findings. No other family member had the same dental problem. Past dental history revealed that she had got composite veneering done in her upper and lower anterior teeth by some local dentist one and a half year back but since then frequent chipping of composite veneering in upper and lower anteriors has occurred so the patient was dissatisfied and disillusioned with dental treatment. Also there were multiple diastemas between maxillary teeth which were not addressed by earlier dentist. (Fig. 1a)
 | Fig. 1a Showing Chipping Of Composite Veneering In Upper And Lower Anteriors ; Presence Of Multiple Diastemas.
 |
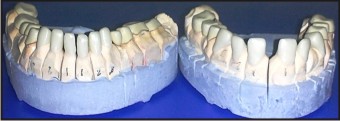
Patient also had crowding in lower teeth associated with deep bite and hypoplastic posteriors. (Fig. 1b and Fig. 1c). After thorough examination, the patient was diagnosed as having a hypoplastic type of amelogenesis imperfecta.
 | Fig. 1b Showing Lower Anterior Crowding And Hypoplastic Lower Posterior Teeth.
 |
 | Fig. 1c Showing Malformed Upper Molars
 |
The treatment started with complete oral prophylaxis with oral hygiene instructions. Maxillary right second molar was extracted since it was grossly decayed and mandibular left first premolar was extracted since it was out of arch.
After 15 days, maxillary and mandibular complete arch impressions were made using alginate. Diagnostic casts were poured using type III dental stone. Face-bow transfer was done (Fig. 2a and Fig. 2b) and interocclusal records were made to mount the casts in centric relation on a semi-adjustable articulator.
 | Fig. 2a Showing Face-bow Transfer Using Slidematic Face Bow.
 |
 | Fig. 2b Showing Face-bow Transfer Using Slidematic Face Bow.
 |
In treatment planning special attention was given to improve the aesthetics and function. Fabrication of metal-free crowns for the maxillary and mandibular anterior teeth and metal-ceramic crowns for posterior teeth was planned.
The patient was informed of the diagnosis, the treatment planned and her consent was taken before the start of the procedure. As the patient had 5 to 6 mm of interoccluslal distance, the vertical dimension was raised around 1.5-2.0 mm. An Occlusal splint was fabricated to evaluate the patient to altered VDO and patient was kept for observational phase of 6 weeks. The patient was instructed to wear the splint all the time, except during teeth cleaning. She was compliant during a 6-week evaluation period. The patient tolerated increased OVD with no sign or symptoms of muscle soreness or TMJ pain. In the meantime, those teeth requiring endodontic treatment underwent root canal therapy.
The diagnostic tooth preparation and diagnostic wax patterns were completed on the mounted casts at planned OVD. The diagnostic wax up models were duplicated and another set of casts were produced to form a template which was used to determine necessary tooth reductions, adequacy of tooth preparation design, and the first set of acrylic provisionals.
Tooth preparations for metal-free anterior crowns and metal-ceramic posterior crowns were completed. Gingival tissues were retracted (Fig. 3). Final impressions were made with polyvinyl siloxane impression material. Provisional crowns already made from the diagnostic wax-up template tried for esthetics and phonetics requirement; checked in for margins, proximal contacts and occlusion and cemented with provisional cement. Then, we made another impression of these provisional restorations which was sent to the lab for duplication of contours in final restorations.
 | Fig. 3 Showing Prepared Upper Teeth With Gingival Displacement Done
 |
The maxillary cast was mounted on an articulator using face bow transfer. And mandibular cast was mounted in centric relation using inter-occclusal recording material.
The articulator was sent to the lab for the fabrication of zirconia copings for anterior metal-free crowns and metal copings for posterior metal-ceramic crowns (Fig. 4). Coping trial for zirconia copings as well as metal copings was done and a new bite registration was done using aluwax to verify earlier jaw relation record. Later metal-free crowns and metal-ceramic crowns were fabricated; tried in, margins, proximal contact and occlusion checked. Right and left Canine guided occlusion (Fig. 5a and Fig. 5b) and anterior guidance (Fig. 5c) was developed. Finally, the provisional crowns were replaced by metal-free crowns in the anterior teeth and porcelain fused to metal crowns in the posterior teeth. These crowns were cemented using dual cure resin cement. Excess cement was removed and finishing of the margins was done using finishing stones.
 | Fig. 4 Showing Fabricated Zirconia Copings For Anterior Teeth And Metal Copings With Opaque Porcelain On Posterior Teeth.
 |
 | Fig. 5a Showing Left And Right Canine Guidance
 |
 | Fig. 5b Showing Left And Right Canine Guidance
 |
 | Fig. 5c Showing Anterior Guidance
 |
Instructions to Patient
Oral hygiene instructions were reviewed, emphasizing cleaning of the restoration margins. Additional instruction was given on the use of floss threaders and superfloss under the FPD.
Post-treatment Therapy
The patient was seen at 1- and 2-week follow-up appointments (Fig. 6a and Fig. 6b). The patient stated that she was pleased with esthetics, function, and comfort of the prostheses. Oral hygiene was excellent. The patient was given instructions to seek 6- month prosthodontic and periodontic recall appointments.
 | Fig. 6a Postoperative View With Functionally And Esthetically Restored Teeth.
 |
 | Fig. 6b Postoperative View With Functionally And Esthetically Restored Teeth.
 |
Prognosis
The patient was very motivated and dedicated to restoring her oral health to optimal condition. Her positive attitude and improved oral hygiene should help to ensure a favourable prognosis. Long-term prognosis will depend on consistent and continued good oral hygiene practice.
Conclusion
In cases where the esthetics and function of teeth have been compromised as a result of amelogenesis imperfecta, thorough diagnosis and treatment planning are essential to achieve a satisfactory esthetic and functional result. The treatment plan for treating a case with amelogenesis imperfecta is related to many factors including age of the patient, socioeconomic status, type and severity of the disorder. This clinical report described the oral rehabilitation of a female patient affected by hypoplastic amelogenesis imperfecta.
The treatment of choice using the metal-free crowns for anterior teeth and the porcelain fused to metal crowns for the posterior teeth was efficient for achieving esthetic and functional rehabilitation. At the end of the treatment, the patient was very pleased with the result.
References
1. Neville BW, Douglass DD, Allen CM, Bouquot JE. Abnormalities of teeth. In: Oral and Maxillofacial Pathology. 2nd ed.. Pennsylvania:Elsevier;2004. 89-94.
2. Shafer, Hine, Levy. Shafer’s textbook of oral pathology, 6th ed. Delhi, India: Elsevier; 2009.
3. Peter JM Crawford, Michael Aldred and Agnes Bloch-Zupan. Amelogenesis imperfect.Orphanet Journal of Rare Diseases 2007.
4. Encinas RP, Garcia-Espona I, Mondelo JMNR. Amelogenesis imperfecta: Diagnosis and resolution of a case with hypoplasia and hypocalcification of enamel, dental agenesis, and skeletal open bite.Quintessence Int 2001;32:183–189.
5. Coffield KD, Phillips C, Brady M, Roberts MW, Strauss RP, Wright JT (2005) The psychosocial impact of developmental dental defects in people with hereditary amelogenesis imperfecta. J Am Dent Assoc 136:620–630
6. Witkop CJ Jr. Amelogenesis imperfecta, dentinogenesis imperfecta and dentin dysplasia revisited: Problems in classification. J Oral Pathol 1988; 17:547–553.
7. Aldred MJ, Crawford PJM. Variable expression in amelogenesis imperfecta with taurodontism. J Oral Pathol 1988;17:327–333.
8. William WP, Becker LH. Amelogenesis imperfecta: functional and esthetic restoration of severly compromised dentition. Quintessence Int 2000;31: 397-403.
9. Collins MA, Mauriello SM, Tyndall DA, Wright JT. Dental anomalies associated with amelogenesis imperfecta: A radiographic assessment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1999;88:358–364.
10. Witkop CJ Jr. Partial expression of sex-linked amelogenesis imperfecta in females compatible with the Lyon hypothesis. Oral Surg Oral Med Oral Pathol 1967;23:174-82.
11. Mayur Chaudhary, Shweta Dixit1, Asha Singh2, Sanket Kunte. Amelogenesis imperfecta: Report of a case and review of Literature. JOMFP: Vol. 13 Issue 2 Jul - Dec 2009
12. Lyon MF. Gene action in the X-chromosome of the mouse (Musmusculus L.). Nature 1961;190:372-3.
13. Lyon MF. Sex chromatin and gene action in the mammalian X-chromosome. Am J Hum Genet 1962;14:135-8.
14. Crawford PJM, Aldred MJ: X-linked amelogenesis imperfecta: presentation of two kindreds and a review of the literature. Oral Surg Oral Med Oral Pathol 1992, 73:449-455.
15. Robinson FG, Haubenreich JE. Oral rehabilitation of a young adult with hypoplastic amelogenesis imperfecta: A clinical report. J Prosthet Dent 2006; 95:10–13.
16. Siadat H, Alikhasi M, Mirfazaelian A. Rehabilitation of a patient with amelogenesis imperfecta using all-ceramic crowns: A clinical report. J Prosthet Dent 2007;98:85–88.
17. Y. Bharath Shetty • Akshay Shetty. Oral Rehabilitation of a Young Adult with Amelogenesis Imperfecta: A Clinical Report. J Indian Prosthodont Soc (Oct-Dec 2010) 10(4):240–245.
18. Kingsley H.C. Chan, Edward H.T. Ho, Michael G. Botelho, Edmond H.N. Pow. Rehabilitation of amelogenesis imperfecta using a reorganized approach: A case report. Quintessence Int 2011;42:385–391
19. Ilione Kruschewsky Costa Sousa Oliveira Jussara de Fátima Barbosa Fonseca, Flavia Lucisano Botelho do Amaral, Vanessa Gallego Arias Pecorari, Roberta Tarkany Basting, Fabiana Mantovani Gomes França. Diagnosis and esthetic functional rehabilitation of a patient with amelogenesis imperfect. Quintessence Int 2011;42:463–469)
|